Research Article - (2018) Volume 2, Issue 1
Doson Chua*
Pharmacy Department, St Paul’s Hospital, Vancouver, Canada
*Corresponding Author:
Doson Chua
Pharmacy Department
St Paul’s Hospital, 1081 Burrard Street
Vancouver, BC V6Z 1Y6 Canada
Tel: 604-806-8153
E-mail: dchua@providencehealth.bc.ca
Received Date: December 29, 2017; Accepted Date: January 08, 2018; Published Date: January 15, 2018
Citation: Chua D (2018) Use of Non-vitamin K Antagonist Oral Anticoagulants (NOAC) for Stroke Prevention in Patients with Atrial Fibrillation and Underlying Valvular Heart Disease: A Systematic Review. Cardiovasc Invesfig. Vol.2 No.1:1
Background: Non-vitamin K antagonist oral anticoagulants (NOACs) are commonly used for stroke prophylaxis in patients with atrial fibrillation (AF), but their efficacy and safety in patients with underlying valvular heart disease (VHD) is unknown. Methods: A search of MEDLINE, CENTRAL, Embase, clinicaltrials.gov was performed with the terms direct oral antiocoagulants, new oral anticoagulants, DOAC, NOAC, rivaroxaban, apixaban, dabigatran, valvular heart disease, aortic stenosis, aortic regurgitation, mitral regurgitation, tricuspid stenosis, tricuspid regurgitation, pulmonary stenosis and pulmonary regurgitation. Only clinical studies with clinical endpoints that compared NOACs with warfarin in patients with AF and identified VHD were included. Results: Four clinical studies were retrieved based on our search criteria. Subgroup analysis of the landmark trials comparing a NOAC to warfarin in AF patients with underlying VHD demonstrated that NOACs had similar or superior efficacy in stroke prevention compared to warfarin. The risk bleeding with NOACs compared to warfarin in these patients yielded inconsistent results. Conclusion: Based on the available evidence, NOACs provide similar or superior stroke reduction compared to warfarin in patients with AF and VHD, especially in aortic valve disease and mitral regurgitation. The rate of major bleeding between NOACs and warfarin in this patient population is unclear. Keywords: Non-vitamin K antagonist oral anticoagulants; Heart disease; Atrial fibrillation; Mitral regurgitation; Tricuspid regurgitation
Keywords
Non-vitamin K antagonist oral anticoagulants; Heart disease; Atrial fibrillation; Mitral regurgitation; Tricuspid regurgitation
Introduction
Atrial fibrillation (AF) is a commonly encountered medical condition and its prevalence is increasing, especially with an aging population. Patients with AF have a four-fold increase in the risk of stroke compared to patients in sinus rhythm [1]. The use of oral anticoagulation reduces the risk of stroke by approximately 60% and is substantially more effective than antiplatelet therapy [2]. Warfarin, a vitamin K dependent oral anticoagulant, has been well proven to reduce the risk of stroke in AF and is the first line anticoagulant used for many decades [3]. However, warfarin is a difficult anticoagulant to use given its variable kinetics. Its anticoagulant effect is influenced by external factors such as diet, concomitant drug interactions and concomitant illnesses. It is estimated that only 50% of patients on warfarin are within their therapeutic international normalized ratio (INR) and thus, are commonly under- or over-anticoagulated [4].
Non-vitamin K antagonist oral anticoagulants (NOAC) such as dabigatran, rivaroxaban and apixaban, have been introduced and provides another option for anticoagulation in patients with AF. The pharmacokinetic profiles of NOACs are much more favorable compared to warfarin, as they possess predictable kinetics and are less influenced by diet and drug interactions. This leads to more predictable and stable anticoagulation. Several landmark trials have shown that NOACs are similar or superior to warfarin anticoagulation for AF and that some NOAC agents demonstrate less bleeding [5-7]. This has led to the increased use of NOACs for anticoagulation in AF given its ease of use and superior clinical outcomes compared to warfarin. Current AF guidelines recommend the use of NOACs over warfarin for stroke prevention in non-valvular AF based on landmark clinical trials [8].
As the presence of valvular pathologies with AF carries a higher stroke risk and the CHADS2 stroke risk score would not be applicable to such patients, the landmark NOAC trials excluded patients in AF with known underlying valvular heart disease (VHD). This has led to the development of the terms “nonvalvular AF” and “valvular AF” in the literature. Only recently has there been a clear definition of non-valvular AF in the guidelines, with the US and Canadian guidelines specifying that non-valvular AF is AF occurring in the absence of rheumatic mitral stenosis (MS) or bioprosthetic or mechanical heart valves [9,10]. It is not known if NOACs still provide superior stroke reduction compared to warfarin in AF patients with underlying VHD, excluding MS and prosthetic heart valves. As the prevalence of VHD increases in the general population and with age, more patients are likely to have underlying native VHD in addition to AF. The concomitant presence of AF and native VHD can influence decisions on the type of anticoagulant to use in these patients. The objective of this systematic review is to determine the efficacy and bleeding risks of NOACs compared to warfarin in patients with AF and underlying native VHD (excluding mitral stenosis and prosthetic valve disease).
Materials and Methods
A search of MEDLINE, CENTRAL, Embase, clinicaltrials.gov was performed from January 2008 to October 2017 with the search terms direct oral anticoagulants, new oral anticoagulants, DOAC, NOAC, rivaroxaban, apixaban, dabigatran, valvular heart disease, aortic stenosis, aortic regurgitation, mitral regurgitation, tricuspid stenosis, tricuspid regurgitation, pulmonary stenosis and pulmonary regurgitation. The limits to the search were English language journals and studies limited to humans and clinical endpoints. In addition, a manual search of references of identified articles and of the similar articles suggested by the databases was performed.
The criteria for inclusion of the study in our review were randomized controlled trials and observational trials. Systematic reviews, meta-analysis, editorials, narrative reviews and commentaries were excluded. Only trials with clinical efficacy endpoints (stroke, systemic embolism, death) and clinical safety endpoints (bleeding, major bleeding, minor bleeding and life threatening bleeding, intracranial hemorrhage) were included. The studies must have compared a NOAC versus warfarin in a study population of patient with AF and underlying VHD. The trials retrieved for review were reviewed independently by the 2 authors (ST, DC) for inclusion into this review.
Results
Based on our search parameters, 33 publications were identified (Figure 1). After ensuring the publications met the inclusion and exclusion criteria, 28 publications were removed. This resulted in 5 studies that met our inclusion criteria and were retrieved for review [11-15]. There were two publications that retrospectively analyzed the same subgroup of patients with VHD from the ROCKET AF trial by the same authors [12,15]. The Breithardt et al. paper was excluded as it sub-analyzed outcome data from the ROCKET AF trial (patients with VHD) and then further sub-analyzed these outcomes based on the specific valve pathology [15]. Thus, the authors were further sub-analyzing data they previously analyzed from ROCKET AF. Based on search methodology described, 4 publications were included in this systematic review (Table 1).
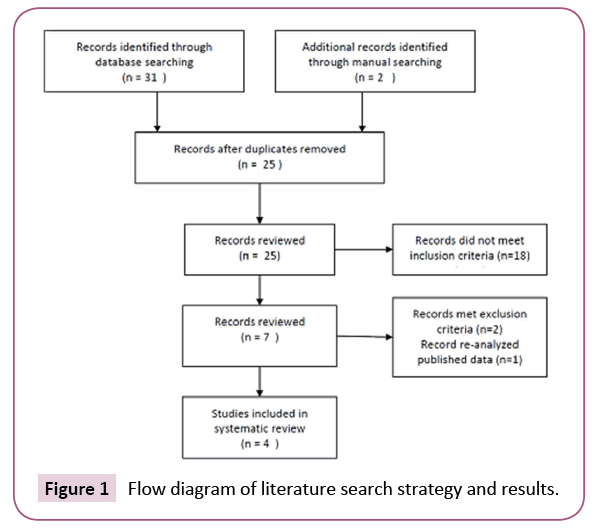
Figure 1: Flow diagram of literature search strategy and results.
Table 1. Summary of studies included in systematic review of NOACs versus warfarin in patients with AF and VHD.
| Study | Study Design | Patient Population | NOAC | Comparator | Efficacy Outcome | Safety Outcome |
|---|---|---|---|---|---|---|
| Ezekowtiz et al. [11] | Post hoc analysis of RELY randomized controlled trial | N = 3,950 patients with AF CHADS2 > 1 and VHD MR=78% AR = 20% TR = 29% AS = 12% MS = 4.8% |
Dabigatran 150mg twice a day or Dabigatran 110mg twice a day | Warfarin titrated to an INR 2-3 | Stroke and systemic embolic events Dabigatran 150mg twice a day vs warfarin HR = 0.59; 95% CI [0.37-0.93] Dabigatran 110mg twice a day vs warfarin HR = 0.97; 95% CI [0.65-1.45] | Major bleeding Dabigatran150mg twice a day versus warfarin HR = 0.82; 95% CI [0.64-1.06] Dabigatran 110mg twice a day versus warfarin HR = 0.73; 95% CI [0.56-0.95] |
| Breithardt et al. [12] | Post hoc analysis of ROCKET AF randomized controlled trial | N= 1,992 patients with AF CHADS2>2 and VHD MR = 89% AR = 24.8% AS =11% |
Rivaroxaban 20mg daily (15mg daily if GFR 30-40ml/min) |
Warfarin titrated to an INR 2-3 | Rivaroxaban versus warfarin HR = 0.83; 95% CI [0.55-1.27] |
Rivaroxaban versus warfarin HR = 1.25; 95% CI [1.05-1.49] |
| Avezum et al. [13] | Post hoc analysis of ARISTOTLE randomized controlled trial | N= 4,808 patients with AF CHADS2>1 and VHD MR = 74.5% MS = 2.7% AR = 18.4% AS = 8% |
Apixaban 5mg twice a day (2.5mg twice a day if age> 80 years, weight < 60kg or Creatinine > 133mmol/L) |
Warfarin titrated to an INR 2-3 | Stroke or systemic embolism Apixaban versus warfarin HR = 0.70; 95% CI [0.51-0.97] |
Major bleeding (ISTH bleeding) Apixaban versus warfarin HR = 0.79; 95% CI [0.61-1.04] Major or clinically relevant non-major bleeding Apixaban versus warfarin HR = 0.77; 95% CI [0.64-0.93] |
| Noseworthy et al. [14] | Retrospective cohort study comparing NOAC versus warfarin using administrative database | N= 20,158 patients being treated with a NOAC (dabigatran, rivaroxaban, apixaban) for AF with VHD | Dabigatran, rivaroxaban or apixaban | Matched with warfarin (titrated INR 2-3) patients | Stroke or systemic embolism NOAC versus warfarin HR = 0.76; 95% CI [0.59-0.98] |
Major bleeding NOAC versus warfarin HR = 0.84; 95% CI [0.72-0.97] |
MR: Mitral regurgitation, MS: Mitral stenosis, AR: Aortic regurgitation, AS: Aortic stenosis, TR: Tricuspid regurgitation, VHD: Valvular heart disease, NOAC: Non-vitamin K oral anticoagulant, INR: International normalized ratio, AF: Atrial fibrillation
Ezekowitz et al. concluded a post hoc analysis of the RE-LY trial comparing dabigatran (at doses of 150 mg and 110 mg twice a day) compared to warfarin in AF patients who were classified as having VHD of the 18,113 patients in the RE-LY trial, there were 3,950 patients enrolled with any VHD. A significant portion of patients with VHD in the RE-LY had MR (mitral regurgitation) [11]. Dabigatran 150 mg twice demonstrated superior reduction in stroke and systemic embolism as compared to warfarin with no difference in bleeding. Dabigatran 110 mg twice demonstrated no difference in the efficacy endpoint of stroke or systemic embolism compared to warfarin, but had significantly less major bleeding. The authors also conducted a test of interaction with the presence of VHD on the efficacy and safety outcome between the dabigatran and warfarin group in this post hoc analysis. The presence of VHD did not influence the efficacy outcome in the dabigatran group (150 mg and 110 mg doses) compared to warfarin (interaction p=0.63 for dabigatran 150 mg group and interaction p=0.65 for dabigatran 110 mg group). The authors concluded that presence of VHD did not influence the comparison of dabigatran with warfarin in the RE-LY trial in regards to efficacy and bleeding outcomes.
Briehardt et al. conducted a post-hoc analysis of the ROCKET AF trial which evaluated rivaroxaban compared to warfarin in AF patients with VHD [12]. MR was the most frequent VHD present in this study population. There were 1,992 patients with AF and VHD in the overall ROCKET AF trial of 14,171 patients. The rates of stroke or systemic embolism were similar between rivaroxaban and warfarin. The rates of major bleeding or non-major clinically relevant bleeding (NMCR) was higher in the rivaroxaban group as compared to warfarin. When the presence of VHD was analyzed to determine if there was an influence on the efficacy outcome as compared to patients with no VHD, no interaction of VHD was found (p value for interaction of VHD=0.76). When the presence of VHD was analyzed to determine if it influenced major and NMCR bleeding outcomes, an interaction was identified (p value for interaction of VHD=0.034). Based on these results, the authors concluded that in patients with AF and VHD, rivaroxaban provided similar stroke prevention benefits as compared to warfarin but is associated with a higher risk of bleeding.
Avezum et al. evaluated the use of apixaban in patients with AF and VHD based on a post-hoc analysis of the ARISTOTLE trial of the 18,201 patients enrolled in ARISTOTLE, 4,808 patients had documented VHD [13]. MR and aortic regurgitation (AR) was the most common valve pathologies identified. The apixaban group had lower rates of stroke or systemic embolism as compared to the warfarin group, similar to the overall ARISTOTLE trial results. The p value for the VHD interaction in respect to the efficacy outcome was not statistically significant (p=0.378). The rate of International Society of Thrombosis and Haemostasis (ISTH) major bleed was not different between the apixaban and warfarin group, however the rates of major or clinically relevant nonmajor bleeding was lower in the apixaban group as compared to warfarin. There was no interaction of VHD on the safety outcome of ISTH major bleeding or major or clinically relevant non-major bleeding (p value for interaction=0.228 and 0.121 respectively). The authors concluded that there was no evidence of a differential effect of apixaban over warfarin in reducing stroke or systemic embolism in AF patients with or without VHD.
Noseworthy et al. conducted a retrospective analysis of an administrative claims database to determine the benefit and safety of NOACs as compared to warfarin in patients with AF and VHD [14]. They identified 20,158 patients with AF and VHD (post-surgical valve repair or replacement) or native VHD who received warfarin, dabigatran, rivaroxaban or apixaban between Oct 1 2010 to April 30 2015. The vast majority of patients derived from this database had MR, aortic stenosis (AS) or AR (19,351 patients). There were very few patients with mitral stenosis (MS) or post-surgical valve disease, thus analysis of these groups was not performed by the authors. The rate of stroke or systemic embolism was lower in the NOAC group as compared to the warfarin group. Similarly, the rate of major bleeding was lower in the NOAC group versus the warfarin group. The authors conclude that NOACs can be used in patients with AF and VHD and may even be preferable over warfarin. However, the authors acknowledge that the largest limitation of this study was its retrospective nature.
Discussion
The use of NOACs in patients with AF is well established and NOACs are currently recommended over the use of warfarin. Whether NOAC provide superior benefit in stroke prevention over warfarin in patients with AF and VHD is less clear. A systemic review of the available evidence consistently demonstrates that NOACs provide similar or superior stroke reduction compared to warfarin in AF patients with VHD, however several questions still remain.
One barrier in determining if NOACs are superior to warfarin in patients with valvular AF is that the definition of non-valvular AF is inconsistent and not universally defined. The exclusion criteria for the landmark NOAC trials used varying definitions of valvular AF (Table 2). This lack of universal definition of non-valvular AF has led to continued debate regarding which patients with AF and underlying VHD should be treated with a NOAC. MR was the most common valvular lesion in patients with VHD enrolled in the landmark NOAC trials.
Table 2. Exclusion criteria from landmark clinical trials comparing NOAC to warfarin in atrial fibrillation.
| Trial | NOAC | Exclusion Criteria |
|---|---|---|
| RE-LY | Dabigatran | History of heart valve disorder (i.e., prosthetic valve or hemodynamically relevant valve disease) and significant mitral stenosis |
| ROCKET AF | Rivaroxaban | Hemodynamically significant mitral valve stenosis, prosthetic heart valves (annuloplasty with or without prosthetic ring, commissurotomy and/or valvuloplasty is permitted) |
| ARISTOTLE | Apixaban | Clinically significant moderate or severe mitral stenosis and prosthetic heart valves |
The benefit of NOACs over warfarin in stroke reduction in AF patients with VHD (valvular AF) is consistent between the studies analyzed above. The results of these post-hoc studies are similar to the results of the overall NOAC trial from which they were derived from. Subgroup analysis of patients with AF and VHD in the RE-LY study showed that dabigatran 150 mg was superior to and 110 mg was similar to warfarin in stroke prophylaxis. These results were similar in the overall patient population of the RE-LY trial. Similarly, post-hoc analysis of patients in the ROCKET AF trial with AF and VHD showed that rivaroxaban 20 mg daily provided a similar effect of stroke prophylaxis compared to warfarin. The overall ROCKET AF study showed that rivaroxaban 20 mg daily was non-inferior to warfarin in stroke prevention. Post-hoc analysis of the patients with AF and VHD in the ARISTOTLE trial revealed that apixaban was superior to warfarin in stroke prevention. This is consistent with the results of the overall ARISTOTLE trial which also demonstrated that apixaban was superior to warfarin. This subgroup, post-hoc analysis of the landmark NOAC trials are the best evidence available which supports the use of NOAC in patients with AF and VHD. The retrospective cohort study by Noseworthy et al. also provides a similar finding of NOACs being superior to warfarin with less rates of major bleeding. The most recent American College of Cardiology valvular heart disease guidelines, which recommends NOACs be used in preference over warfarin in patients with AF and VHD (specifically aortic valve disease, tricuspid valve disease or MR) are largely based on the studies described above [10]. The evidence for use of NOACs in patients with MS is unclear as very few patients with MS were identified in the landmark NOAC studies. As well, patients with prosthetic valves were largely absent from the subgroup analysis of the VHD patients in the landmark NOAC studies. Thus, use of NOACs in patients with AF and MS or prosthetic valves should be discouraged due to lack of data.
The risk of major bleeding in patients with AF and VHD treated with NOACs compared to warfarin is less clear. Post-hoc analysis of the ROCKET AF trial showed that rivaroxaban had statistically significant higher rates of major bleeding compared to warfarin. Patients with AF and VHD in the RE-LY and ARISTOTLE studies had similar or less rates of major bleeding with dabigatran or apixaban compared to warfarin. It is unclear why rivaroxaban is the only NOAC to suggest a possible increased risk of bleeding in these post-hoc analyses. This is contrary to the overall ROCKET AF study which showed that rivaroxaban had less major bleeding compared to warfarin.
The biggest limitation to our analysis is that all the available evidence is based on post-hoc study data or is retrospective in nature. The number of patients with AF and VHD in the landmark NOAC trials is quite small and would not provide adequate power to detect a true benefit of NOACs over warfarin. As well, the definitions of major bleeding varied between the above studies, making firm conclusions regarding safety more difficult. As well, patient co morbidities and underlying valvular pathologies varied between the studies above, making generalizations of results less clear.
Conclusion
Based on the best available evidence, NOACs demonstrate similar or superior stroke reduction in patients with AF and VHD as compared to warfarin. The most current guidelines support this conclusion by recommending NOACs over warfarin in patients with AF and VHD, specifically MR, AS and AR. The evidence suggests that rivaroxaban may be associated with a higher rate of major bleeding compared to warfarin while dabigatran and apixaban shows less major bleeding.