- (2011) Volume 12, Issue 4
Verity R Sutton, Michael KY Hong, Peter R Thomas
Department of Surgery, Northeast Health. Wangaratta, Australia
Received March 5th, 2011 - Accepted April 19th, 2011
Context Post-ERCP pancreatitis is the most common complication of endoscopic retrograde cholangiopancreatography (ERCP). A simple method of predicting patients who are at risk of developing post-ERCP pancreatitis is needed to allow those at low risk to be discharged on the same day of their procedure. The aim of this study was to confirm that 4-hour post-ERCP serum amylase level is predictive of post-ERCP pancreatitis. Patients A study of 886 ERCPs performed at a single centre was conducted. Main outcome measure Four-hour amylase level was recorded, along with patient demographics, procedural details, presence of pancreatogram, and morbidity and mortality. Results Pancreatitis occurred in 4.4% of ERCPs. Hyperamylasaemia was found to be predictive of post-ERCP pancreatitis, with other risk factors being a younger age and pancreatogram. Hyperamylasaemia was also predictive of post-ERCP pancreatitis in the subgroup of patients who had undergone pancreatogram. Conclusions The 4-hour amylase level is a useful measure in the prediction of post-ERCP pancreatitis. Patients who have undergone pancreatogram should be admitted if 4- hour amylase level is greater than 2.5 times the upper limit of reference. Patients who have not undergone pancreatogram should be admitted if 4-hour amylase level is greater than 5 times the upper limit of reference.
Amylases; Cholangiopancreatography, Endoscopic Retrograde /complications; Pancreatitis
ULR: upper limit of reference
Endoscopic retrograde cholangiopancreatography (ERCP) has evolved from a difficult diagnostic test into a useful but complex therapeutic procedure [1]. Although it is still associated with the highest morbidity of all common endoscopic procedures, like many other procedures, there is a growing trend towards same-day admission and discharge.
A key issue in determining which patients are safe for same-day discharge is predicting who will develop post-ERCP pancreatitis, the most common complication [2, 3, 4, 5, 6, 7, 8, 9]. Early determination would allow timely coordination of overnight admission and prompt initiation of appropriate supportive therapies for the patients at risk, and safe discharge of others. Clinical assessment alone is unreliable, as post-ERCP pancreatitis frequently presents late [10].
Numerous studies have been conducted to elucidate factors that may enable the endoscopist to predict post-ERCP pancreatitis. One of the more practical tests to emerge is post-ERCP amylase level. Although hyperamylasaemia is a common and often benign phenomenon after ERCP, it has been shown consistently to be associated with post-ERCP pancreatitis [10, 11, 12, 13, 14, 15, 16, 17, 18, 19].
A practical algorithm was proposed in an earlier study by the senior author, where patients could be discharged on the same day based on the 4-hour post- ERCP amylase level. The aim of our study was to reevaluate this algorithm and to improve it using greater numbers and to explore other potentially useful factors such as age, gender and pancreatogram.
A retrospective study was carried out on all elective and emergency ERCP performed at a single rural centre in Victoria, Australia, between August 1997 and December 2009. The age of patients ranged from 16 to 98 years. All procedures were carried out by a single operator (P.R.T.), who has ERCP training recognised by the Conjoint Committee for the Recognition in Training in Gastrointestinal Endoscopy. Exclusion criteria included pre-existing pancreatitis within two weeks prior to ERCP and lack of post-procedure amylase levels.
All procedures were conducted under sedation or general anaesthesia, using a side-viewing duodenoscope (Olympus Australia, Mt Waverley, VIC, Australia). Most ERCP were planned as day procedures unless patient factors dictated otherwise. Patients received standard peri-operative treatment including i.v. fluids and prophylactic antibiotics. All patients had serum amylase measured 4 hours postoperatively and were admitted overnight if levels were greater than 3 times the upper limit of reference (3 ULR) or when there were any clinical concerns, in accordance with the algorithm devised previously by Thomas and Sengupta [19]. Clinical concerns included uncontrolled pain, inability to tolerate diet, and emergency patients with ongoing sepsis.
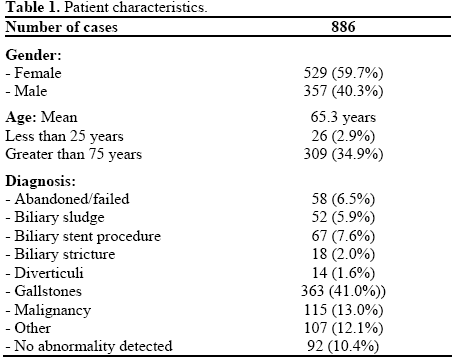
All results were recorded prospectively including patient demographics (Table 1), procedural details, presence of pancreatogram, 4-hour amylase level, morbidity and mortality. This also included patients where biliary cannulation was not attempted or had failed. The amylase levels were standardised due to changes in the reference ranges over the study period. Definitions of complications were based on those described by Cotton et al. [20]. Pancreatitis was defined as abdominal pain persisting for at least 24 hours associated with an amylase level of at least 3 times the ULR, with CT scan used when the diagnosis was uncertain. This was further categorised into mild pancreatitis, requiring hospitalisation for less than 3 nights; moderate for 4-9 nights; and severe for 10 or more nights, ICU admission, or the development of local or systemic complications.
All data were recorded in an Excel spreadsheet and the statistical analysis was carried out using Statistical Package for the Social Sciences (SPSS) 18. Mean, standard deviation (SD), 95% confidence interval (95% CI), range and frequencies were used as descriptive statistics. To determine if post-ERCP amylase levels were normally distributed, log transformation was applied before plotting the values and applying the Shapiro-Wilk test. This showed that the levels for those who did not develop post-ERCP pancreatitis were normally distributed, but not for those who developed post-ERCP pancreatitis. Therefore, the Mann-Whitney- U test was used for all statistical testing involving amylase levels. The Fisher’s exact test and the liner-bylinear association chi-squared were used for the contingency tables. Likelihood ratio was computed in order to test the strength of a diagnostic test [21]. Likelihood ratio for positive test estimates the odds that a patient who tests positive (i.e. hyperamylasaemia) actually has the disease (pancreatitis). A likelihood ratio greater than 10 indicates a test particularly good for ruling in the disease. Likelihood ratio was calculated according to the following formula: sensitivity / (1 - specificity) [21].
A total of 959 consecutive procedures were carried out during the study period. Of these, 8 (0.8%) patients were excluded as no post-operative amylase was measured, and a further 65 (6.8%) patients were excluded due to pre-existing pancreatitis, giving a total of 886 procedures (92.4%). Of the 886 ERCP studied, 699 were therapeutic (78.9%) and 187 were diagnostic (21.1%). Three hundreds and thirty seven of the ERCP included a pancreatogram (38.0%). All pancreatograms were unintentional and a consequence of the shared anatomy of the ampulla. No attempts at pancreatic duct guide-wire insertion were performed prior to biliary cannulation.
There were 13 deaths in this series (1.5%): 4 of them were related to the procedure (30.8%), the remainder died later from their underlying disease. No deaths were directly related to post-ERCP pancreatitis.
Following the algorithm, only one patient was readmitted for moderate post-ERCP pancreatitis following discharge after ERCP.
In total, 39 patients were diagnosed with pancreatitis (4.4%): 27 mild (69.2%), 9 moderate (23.1%) and 3 severe (7.7%), as defined above. Almost all recovered with in-hospital conservative management, with one patient requiring percutaneous drainage of a pseudocyst, while another eventually died following transfer to a tertiary-referral hospital for further operative management.
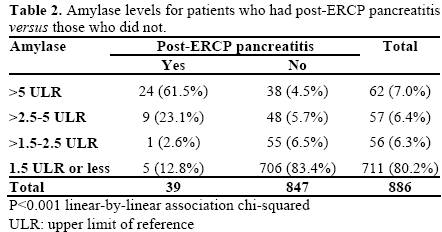
The mean 4-hour amylase for patients with post-ERCP pancreatitis was 9.0 times the ULR (range: 0.46-52.7 ULR) compared with 1.4 times the ULR (range: 0.04- 21.5 ULR) for those without post-ERCP pancreatitis (Table 2). This was statistically significant, demonstrating a clear difference in 4-hour post-ERCP amylase levels between the two groups (P<0.001).
Patients who developed post-ERCP pancreatitis were significantly youger (P<0.001) than patients who did not (54±17 years, range: 19-83 years, vs. 66±17 years, range: 16-98 years). By dividing the data into patients up to age 65 years and over 65 years, it was found that there was an increased frequency of post-ERCP pancreatitis (P<0.001) in the younger group at 7.4% (27/365) vs. 2.3% (12/521) in the older group. There was no significant difference between gender in predicting post-ERCP pancreatitis (26/529, 4.9% in females vs. 13/357, 3.6% in males; P=0.407). Similarly, no statistical difference was found between therapeutic and diagnostic ERCP (27/699, 4.0% vs. 12/187, 6.4%, respectively; P=0.168).
A significant association was demonstrated between patients who had a pancreatogram and hyperamylasaemia (2.31±4.47 ULR vs. 1.11±2.29 ULR in no pancreatogram; P<0.001). There was also a significant association (P<0.001) between pancreatogram and the occurrence of post-ERCP pancreatitis, with a prevalence of 8.9% (30 in 337) compared with 1.6% (9 in 549). Furthermore, analysing only the sample of patients who had a pancreatogram, hyperamylasaemia was still positively associated with post-ERCP pancreatitis (9.22±10.13 ULR vs. 1.65±2.63 ULR; P<0.001). In addition, if patients who had pancreatogram were excluded from analysis, hyperamylasaemia was positively associated with post- ERCP pancreatitis (8.69±6.33 ULR vs. 0.99±1.92 ULR; P<0.001).
A receiver-operator characteristic curve was plotted to determine cut-off values for the 4-hour amylase level. Area under the curve was 0.91 (P<0.001 vs. 0.5), demonstrating good test performance. The sensitivity and specificity for amylase levels of 1.5 ULR were 87.2% and 83.4%, for 2.5 ULR they were 84.6% and 89.8%, and for 5 ULR they were 61.5% and 95.5%, respectively. These were taken as practical cut-off values.
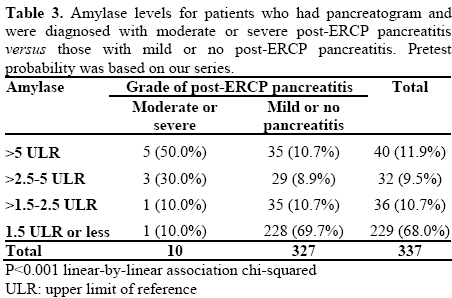
Whilst age was not a practical predictor of post-ERCP pancreatitis, having a pancreatogram and 4-hour amylase clearly were. The data were therefore stratified into those who had pancreatogram and those that did not. Analysis focused on patients who had moderate or severe post-ERCP pancreatitis, as they are most likely to require medical intervention.
For patients who underwent pancreatogram, amylase of 2.5 ULR had a sensitivity of 80.0% and a negative predictive value (NPV) of 99.2% for moderate or severe post-ERCP pancreatitis (Tables 3 and 4). There were just 2 cases of moderate post-ERCP pancreatitis who had an amylase below 2.5 ULR. All cases of severe post-ERCP pancreatitis were above 2.5 ULR.
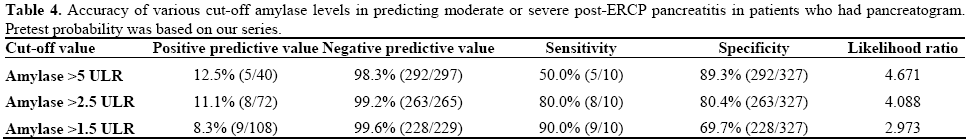
For those without pancreatogram only 2 of 549 (0.4%) patients developed moderate or severe post-ERCP pancreatitis, and both had amylase above 5 ULR (Table 5). Thus amylase above 5 ULR had sensitivity and NPV of 100% (Table 6).
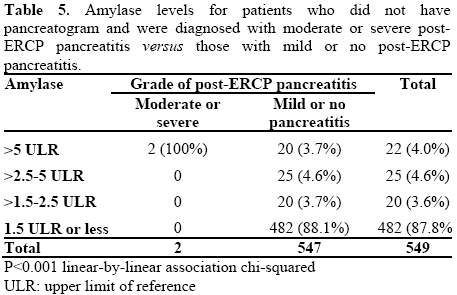
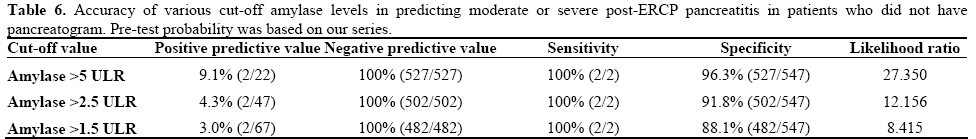
Our study of 959 procedures clearly demonstrates that hyperamylasaemia 4 hours post-ERCP is associated with post-ERCP pancreatitis, and therefore can be used to predict this complication. We established that having a pancreatogram increases the risk of post-ERCP pancreatitis and concluded that hyperamylasaemia is predictive of post-ERCP pancreatitis in both those with and without pancreatograms. From our data, no cases of severe post-ERCP pancreatitis occurred when amylase was below 2.5 ULR, and none below 5 ULR if no pancreatogram was performed.
Although many studies have focussed on determining the most appropriate timing for the post-ERCP amylase level, the 4-hour level appears to have the most support. Post-ERCP amylase has been shown to peak at 90 minutes to 4 hours [14]. Testoni et al. measured the 2-, 4-, 8- and 24-hour amylase level in 409 patients, and found that over two thirds of their patients who were diagnosed with post-ERCP pancreatitis had a 4- hour amylase level greater than 5 ULR, similar to our results (61.5%). They concluded that the 4-hour amylase level minimises the likelihood of underestimating the risk of post-ERCP pancreatitis. Similar observations were made by Christoforidis et al. [11]. More cases of post-ERCP pancreatitis may have been predicted if performance of pancreatogram was considered as a factor in their analyses.
Kapetanos et al. studied amylase levels 2 and 6 hours post-ERCP in 97 patients [13]. They found that amylase greater than 5 ULR at either 2 or 6 hours could both predict post-ERCP pancreatitis with the same accuracy. This appears to be at odds with Ito et al., who found that post-ERCP pancreatitis is frequently associated with a 3-hour amylase greater than 2 ULR that becomes more elevated at 6 hours [12]. This gave a 26% risk of post-ERCP pancreatitis compared with 9% if the 6-hour amylase was decreased. This 6-hour time frame may be impractical for use in determining same-day discharges.
Gottlieb et al. studied the combination of 2-hour amylase, lipase and clinical assessment to predict post- ERCP pancreatitis [10]. They developed an algorithm allowing the discharge of patients with amylase less than 2.4 ULR and lipase less than 4.2 ULR. Unlike amylase levels, the effect of ERCP on lipase levels remains largely unknown. Lipase usually rises later than amylase in pancreatitis and may therefore not be as useful in the early prediction of post-ERCP pancreatitis.
In an earlier study by the senior author on 263 patients, 4-hour post-ERCP amylase level greater than 1.5 ULR was found to be 100% sensitive for post- ERCP pancreatitis [19]. They recommended discharging patients if 4-hour amylase was less than 1.5 the ULR and admitting if it was greater than 3 times the ULR (specificity 95.3%). This algorithm seems more conservative than necessary, as just 6 patients in the current series had post-ERCP pancreatitis with amylase less than 2.5 times the ULR, none of them severe.
Our finding of pancreatogram as an additional risk factor for post-ERCP pancreatitis is certainly not new [4, 11, 19, 22]. In a study comparing contrast media in 1,972 patients, Johnson et al. found that an increased number of pancreatic duct injections resulted in a progressively higher incidence of post-ERCP pancreatitis [23]. It has also been shown that technical factors related to pancreatogram, such as difficult cannulation or pancreatic sphincterotomy, convey additional risk of post-ERCP pancreatitis [22, 24]. These factors were not included in our analysis as the purpose of our study was to validate a simple risk stratification test, rather than to examine all possible contributions to post-ERCP pancreatitis.
Other predictors of post-ERCP pancreatitis have also been studied, including urine amylase [25], urinary trypsinogen activation peptides [26], and trypsinogen-2 [26]. These tests have so far proven to be unhelpful in predicting post-ERCP pancreatitis. Similarly, CRP has been shown to be a late marker for post-ERCP pancreatitis [5], and again, unhelpful in early decisionmaking.
An ideal test for predicting post-ERCP pancreatitis would detect the majority of patients with severe episodes, and would be performed in a timely manner to facilitate same-day discharge. From our results, we propose that patients undergoing ERCP be treated according to whether or not a pancreatogram has been obtained. Patients who have undergone pancreatogram should be admitted if 4-hour amylase level is greater than 2.5 times the ULR. Patients who have not undergone pancreatogram should be admitted if 4-hour amylase level is greater than 5 times the ULR (Figure 1). Nevertheless, if there are other clinical concerns, or if the patient’s social circumstances make a same-day discharge inadvisable, admission may still be necessary in patients with a normal amylase level.
If these criteria were applied to our sample of patients, 10% would be admitted overnight for observation (20% of patients who undergo pancreatogram and 4% of those without a pancreatogram). More than two thirds of post-ERCP pancreatitis and all cases of severe post-ERCP pancreatitis would have been admitted.
We would like to thank Drs. Carolyn Vasey, Matthew Hong, Nancy Suh, and Grace Huang for their assistance in statistical analysis, gathering data, general analysis of the data and preparation of the manuscript. We would also like to thank Ms Julie Day for her help with the literature review. Presented at the “2009 Victorian RACS Annual General Scientific Fellowship Meeting; Lorne, Victoria, Australia. Winner of the “Royal Australasian College of Surgeons D.R. Leslie Prize (2009).
The authors have no potential conflict of interest