Research Article - (2017) Volume 1, Issue 1
Lynn Zaremski* and Ronald Wharton
Department of Cardiology, Montefiore Medical Center, 3444 Kossuth Ave, Bronx, New York
*Corresponding Author:
Lynn Zaremski
Department of Cardiology
Montefiore Medical Center
3444 Kossuth Ave, Bronx, NY 10467
Tel: 917-847-3228
E-mail: lzaremsk@montefiore.org
Received date: 03 June 2017; Accepted date: 24 June 2017; Published date: 30 May 2017
Citation: Zaremski L, Wharton R. Wide Screening of Obstructive Sleep Apnea in a Cardiology Clinic. Cardiovasc Investig. 2017, 1: 1.
Copyright: © 2017 Zaremski L, et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Background: Obstructive sleep apnea (OSA) is widely prevalent, but under-diagnosed. It is not screened for widely. Physicians tend to only screen those they consider at risk. This determination is made either by assessment of body habitus or significant symptoms. Methods: Patients without known OSA at a cardiology clinic were screened using a questionnaire for signs and symptoms of OSA. Patients with high scores were referred for testing. Results: The patient group included 102 patients who obtained OSA testing. Obstructive sleep apnea was highly prevalent in the patients who screened positive, with 84% of patients referred for testing positive for OSA. As OSA became more severe, patients had more comorbidities. Body mass index did not correlate with presence of OSA or severity of OSA. Conclusions: Obstructive sleep apnea is highly prevalent in at risk populations, such as those found in cardiology clinics. Obstructive sleep apnea does not correlate with body habitus, so physician initiated screening for patients with large BMI is not adequate. Wide screening in at risk populations should be employed.
Keywords
Obstructive sleep apnea; Screening; Obesity; Comorbidity
Introduction
Despite increasing awareness, cardiovascular disease remains endemic in America today. Its impact on morbidity and mortality is substantial, as is its great financial burden on the health care system. Patients with cardiovascular disease have an increased incidence of obstructive sleep apnea (OSA).
OSA has been found to increase a patient’s risk of having atrial fibrillation by four fold. In addition, OSA is associated with coronary artery disease, heart failure, and hypertension [1,2].
In recent years, there has been a growing awareness of the epidemic of OSA. Motor vehicle crashes have been estimated to be two to three times more prevalent in patients who suffer from this order as compared to those who do not [3]. In late September 2016, a commuter train crash with fatalities in New Jersey was linked to undiagnosed obstructive sleep apnea in the train’s conductor. It has been reported that sleep apnea may have been the cause of a similar accident on the Long Island Rail Road in early January 2017.
The association between obstructive sleep apnea and obesity is known. Patients who are obese frequently have coexisting cardiovascular illnesses such as hypertension, diabetes, coronary artery disease, and heart failure. Despite the prevalence of these conditions in the outpatient cardiology setting, OSA remains under-diagnosed [4]. In addition, there is very little attention paid to OSA in formal cardiovascular training, and virtually no mention of OSA in guidelines published by the American College of Cardiology for the treatment of various cardiovascular disorders.
Continuous positive airway pressure (CPAP) effectively treats OSA and not only improves potentially dangerous symptoms including daytime sleepiness, but can also improve control of comorbidities including hypertension and atrial fibrillation. Even in patients with resistant hypertension with OSA, CPAP was shown to decrease daytime blood pressure [5]. In patients with atrial fibrillation and OSA, CPAP was shown to decrease recurrence [6].
The gold standard for diagnosis is polysomnography, but this poses a significant barrier to many patients as testing takes place overnight and at a designated center. Polysomnography is used to determine the severity of OSA using the apneahypopnea index (AHI). The AHI is a measure of the severity of OSA and is defined as the average number events per hour of sleep. Home devices to diagnose OSA have recently been approved for use in the United States. They are more convenient for patients and also decrease the cost of diagnosis [7].
Methods
Starting in November 2015, patients at an outpatient cardiology clinic (who were not already diagnosed with OSA) were routinely screened for the presence of obstructive sleep apnea. Upon arrival to the cardiology clinic, patients were offered a questionnaire based on the Berlin Questionnaire and the Epworth Sleepiness Scale (Figure 1). Patients who scored ≥ 2 were offered the opportunity to be tested for the presence of OSA using a device suitable for use in their own home, the WatchPAT (Itamar Medical).
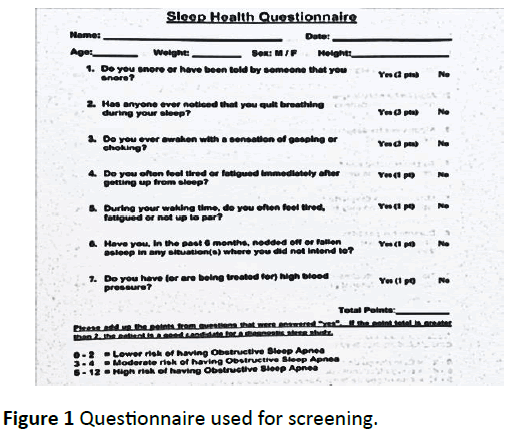
Figure 1: Questionnaire used for screening.
The WatchPAT is approved by the United States Food and Drug Administration for the diagnosis of OSA. It works via peripheral arterial tonometry, and has demonstrated a high degree of correlation compared to the polysomnography, the gold standard [8]. Patients who had abnormal tests (apneahypopnea index (AHI) ≥ 5) were given follow-up with a sleep specialist in order to expedite treatment. Approval from our institutional review board was obtained through a waiver of patient consent for this retrospective study.
Screening for OSA was offered in the interest of optimizing patient care. There was no financial incentive to offer this service, nor was any profit realized from subsequent testing on those patients who were diagnosed with significant OSA.
Patients with scores ≥ 2 were offered home testing through a third party specializing in sleep medicine who also interpreted results. The significance levels were set at 0.05. Baseline characteristics were presented as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables.
The distributions of continuous variables were examined using the Kolmogorov-Smirnov non-parametric test to assess the Normality of the variable distribution. Chi-Square tests and Kruskal-Wallis non-parametric tests were used to assess the OSA severity groups by baseline characteristics. The Spearman correlation was used to assess the relation between BMI and AHI as well as the relationship between the other variables per person and AHI.
A multivariate linear analysis was used to determine the correlation of severity of OSA with the other measured factors. Data were analyzed with SPSS software version 23.0. (SPSS Inc. Headquarters, 233 S. Wacker Drive, 11th floor Chicago, Illinois 60606, USA).
Sleep apnea was defined as absent (AHI <5), mild (AHI 5-15), moderate (AHI 15-30) or severe (AHI ≥ 30). Hypertension was defined as any patient told of a history of this disorder or medications being used to treat hypertension. The presence of systolic heart failure was defined as an ejection fraction reported as ≤ 40%. Diabetes was defined by a history thereof, medications being used to treat this disorder, or glycosylated hemoglobin of ≥ 6.5%. The presence of coronary artery disease was defined as any history of coronary revascularization or angiography demonstrating a stenosis ≥ 70%.
Results
The patient group included 102 patients, 46 (45%) males. The average age was 59.5 ± 11.7 years (Table 1).
Table 1 Baseline characteristics of the patients tested for OSA.
| N(%), mean ± SD | |
|---|---|
| Age | 59.5 ± 11.7 |
| Gender | |
| Male | 46 (45) |
| Female | 56 (55) |
| BMI | 35.2 ± 8.8 |
| AHI | 25 ± 21.7 |
| DM | 58 (57) |
| HTN | 70 (69) |
| Systolic HF | 17 (17) |
| AF | 33 (32) |
| CAD | 20 (20) |
| OSA | |
| Absent | 16 (15.7) |
| Mild | 29 (28.4) |
| Moderate | 24 (23.5) |
| Severe | 33 (32.4) |
Men were more likely to have OSA than women, and this association became more pronounced as severity of disease increased. Patients with moderate or severe OSA were more likely to have HF. Patients were more likely to have hypertension with OSA, but the prevalence of hypertension remained similar among OSA groups (76%, 71%, 73% in mild, moderate, severe OSA, respectively). As severity of OSA worsened, prevalence of CAD significantly increased (Figure 2).
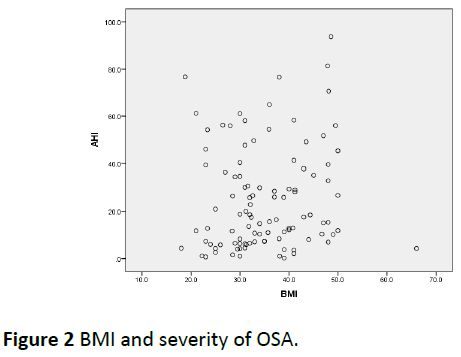
Figure 2: BMI and severity of OSA.
BMI was similar among all OSA groups (Table 2). In a multivariate linear regression, increasing AHI was associated with diabetes and atrial fibrillation. Number of comorbidities increased as OSA severity increased (Table 3 and Figure 3). There was no relationship between AHI and BMI after adjusting for other comorbidities (Table 4).
Table 2 OSA severity and patient characteristics.
| OSA Absent | Mild OSA (N=29) | Moderate OSA (N=24) | Severe OSA (N=33) | p-value | |
|---|---|---|---|---|---|
| AHI | 2.7 ± 1.6 | 9.2 ± 2.6 | 25 ± 13 | 50 ± 16 | <0.001 |
| Age | 57 ± 13 | 57 ± 12 | 60 ± 10 | 62 ± 11 | 0.444 |
| Male | 4(25) | 9(31) | 11(46) | 22(67) | 0.011 |
| BMI | 33 ± 11 | 35 ± 8 | 37 ± 8 | 36 ± 9 | 0.277 |
| DM | 8(50) | 10(34.5) | 12(50) | 28(85) | 0.001 |
| HTN | 7(44) | 22(76) | 17(71) | 24(73) | 0.132 |
| sHF | 1(6.3) | 2(6.9) | 3(12.5) | 11(33) | 0.017 |
| AF | 4(25) | 9(31) | 6(25) | 14(42) | 0.468 |
| CAD | 0 | 3(10) | 6(25) | 11(33) | 0.02 |
Table 3 Number of comorbidities in patient population.
| Number of Comorbidities | Patients, N(%) |
|---|---|
| 0 | 7(6.9) |
| 1 | 29(28.4) |
| 2 | 37(36.3) |
| 3 | 21(20.6) |
| 4 | 8(7.8) |
Table 4 Multivariate linear regression.
| Model 1 | B |
|---|---|
| BMI | 0.219 |
| HTN | 4.052 |
| DM | 14.909 |
| sHF | 10.899 |
| AF | 10.947 |
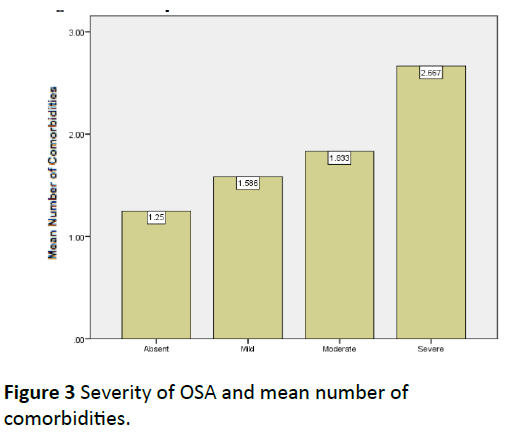
Figure 3: Severity of OSA and mean number of comorbidities.
Baseline characteristics are presented as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables. The distributions of continuous variables were examined using the Kolmogorov-Smirnov non-parametric test to assess the Normality of the variable distribution.
Baseline demographics, comorbidities, and severity of OSA compared by chi square or Kruskal-Wallis non-parametric tests as appropriate. Values are expressed in N(%), mean ± SD. Distribution of number of comorbidities (HTN, AF, sHF, DM and CAD) per patient.
The correlation between BMI and AHI represented by scatterplot. Statistical significance was determined by Spearman correlation.
Histogram of the number of comorbidities by severity of OSA (Absent=AHI<5; Mild=AHI 5-14; Moderate,=AHI 15-29; Severe=AHI ≥ 30).
Discussion and Conclusion
Our findings that OSA was more prevalent in men, in patients with heart failure, and who have coronary artery disease have been previously reported. We also observed that OSA was more common in patients with HTN (69%) and in diabetic patients (57%).
There were two additional findings from this data that we found particularly interesting. The first was the lack of any correlation between BMI and the presence of sleep apnea. This suggests that the widely held notion that a clinician can guess the absence of OSA and degree of severity based on patient’s BMI is invalid. Equally of interest was that there appeared to be a correlation between the number of concomitant co-morbidities that are commonly encountered in the outpatient cardiology arena and the degree of OSA present. Once three simultaneous illnesses were present, the prevalence of severe OSA rose dramatically.
This retrospective analysis of our experience screening patients for OSA was not intended to break any new scientific ground, nor was it designed to suggest any algorithm by which patients could be detected merely by the presence or absence of other illnesses. Its purpose was simply to augment the awareness of how endemic OSA is in society, especially amongst individuals likely to be referred to a cardiology practice. Being methodical about screening may have enormous benefits to the health of our patients and the safety of society.
Potential Conflicts of Interest: after preparation of manuscript, Dr. Ronald Wharton gave a lecture for which he was compensated by Itamar Medical