Keywords
HIV; Gender; India; Stigma; Women living
with HIV; Biopsychosocial model; Intersectionality
Background
With access to effective antiretroviral drug treatment, HIV
infection can now be experienced as a survivable chronic illness,
allowing long-term health management to focus on maintaining
quality of life and infection containment [1,2]. Given the
effectiveness and availability of treatment, it might be assumed
that the stigma experienced by the 2.1 million Indian people
living with HIV (PLH) would be reducing as they receive:
testing and treatment; education about disease management,
virus transmission and life strategies; and social support no
longer constrained by fear of a deadly infection [1,3]. And yet,
stigma has not only survived the advent of antiretroviral drug
treatment in India, but remains pervasive, affecting life patterns
and disrupting biomedical interventions [1,3]. While stigma
is experienced by all PLH, cultural beliefs and unequal power
relations make Indian women particularly vulnerable [4].
In 2014, women represented 41% of Indians diagnosed
with HIV, a percentage that continues to increase [5,6]. The
number of Indian PLH had decreased over the preceding five
years, both in total and among the segments of the population
at greatest risk: sex-workers, men who have sex with men, and
injecting drug users [5,7]. Representing an estimated 1.5 million
persons, these at-risk groups are at the forefront of advocacy
and treatment campaigns [5]. However, this focus, evidenced
for example in preventative educational advertisements [6]
and statistics on advances made in controlling HIV in India
[5], reinforces vernacular perceptions that HIV is on decline,
and is a disease afflicting only people who engage in immoral
behaviours [8]. Over time such associations become accepted
societal truths [8]. Rahangdale et al. reported interviews where
PLH described their fear of being treated as a new kind of
unclean, immoral, social outcast, describing themselves using
the historically caste-laden term untouchable [9], an attitude
and language which has also been found in mainstream media
[10,11]. Yet despite this pervasive cultural association, 90%
of new infections in Indian women do not involve sex-work
[12]. Instead these new infections result from matrimonially
sanctioned sexual relations [13].
Although HIV disease progression is not related to the
biological sex of an individual patient, Indian women’s illness
experience is reported to differ from that of Indian men: for
example, women are 30% less likely to access antiretroviral
drug treatment (ARDT) than men, men are typically diagnosed
at a more advanced stage of the disease, and women experience
greater social stigma than men [3,6,14]. The major factor
limiting regular use of ARDT by women living with HIV (WLH)
is stigma [1,3]. In order to probe for reasons as to the differences
in the experience of being HIV-positive for Indian women and
men, a number of studies utilised sex disaggregated quantitative
data [1,14,15]. The potential risk of this approach is that some
groups of women or men with particular social risk factors
may not be identified if analysis of the data assumes a binary
male: female biological sex paradigm and conflates it with
social constructions of gender (different groups of, and social
conventions about, diverse women and men). For the purposes
of this discussion, an Indian woman’s gender is understood to be formed by the hegemonically defined norms of living within her
particular socially constructed, patriarchal, relational hierarchy,
cultural myths, rituals and folk beliefs. Gender behaviour is
learned via socially sanctioned gender roles, institutional gender
constraints, and norms of behaviour for Indians identifying as a
particular sex. In order to develop care interventions that result
in equitable health outcomes for different groups of women and
men, it is important that manifestations of gendered inequalities
that marginalise particular groups are identified.
Recognising an HIV stigma continum
In examining HIV-related stigma, the reviewed literature
refers to the foundational work of Goffman [16] who defined
stigma as a cultural belief about a social abnormality which
degrades the value of the identity of any individual possessing
that abnormality: in this case the stigmatised person’s value is
degraded through exhibiting an abnormality (HIV infection) to
the socially defined and preferred norm (HIV free) [4,17,18].
Ho and Holloway (2016) identified two cultural beliefs which
are universally mobilised to stigmatise WLH: 1) that being
HIV-positive always indicated immoral behaviour of which
the individual should be ashamed and for which she deserved
to be punished, and 2) that the HIV-positive individual posed
an unmanageable infection risk as she could transmit a disease
understood to be incurable. Ho and Holloway [2] also identified
that manifestations of stigma for WLH could be collated as
public or private via: socio-cultural, relational and psychological
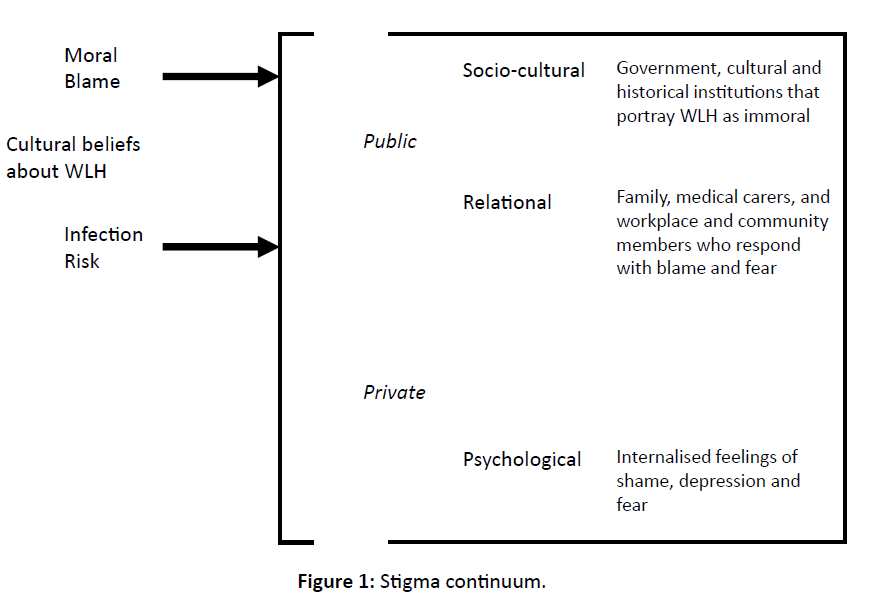
spheres. The information provided by Ho and Holloway [2] is
interpreted diagrammatically here in Figure 1.
Like Ho and Holloway [2], Parker and Aggleton [17] also
noted that in studying PLH, researchers typically separated
private and public life experiences, and prioritised the private
or psychological experience. Such an approach seeks to
understand the PLH psychological experience, and identifies
the need to educate both the uninfected (wider society and
heath care professionals) to be more tolerant, and the infected to
understand their illness, access medical care and develop coping
strategies [1,4,9,13,18]. Parker and Aggleton’s criticism of this
approach is that it ignores Goffman’s insight that stigma is a
public cultural belief, a social construction of degraded identity
where power is wielded to exclude individuals on the basis of
undesirable difference [16]. It is therefore not restricted to the
psychological realm, but compromises social functioning and
all inter-human relationships.
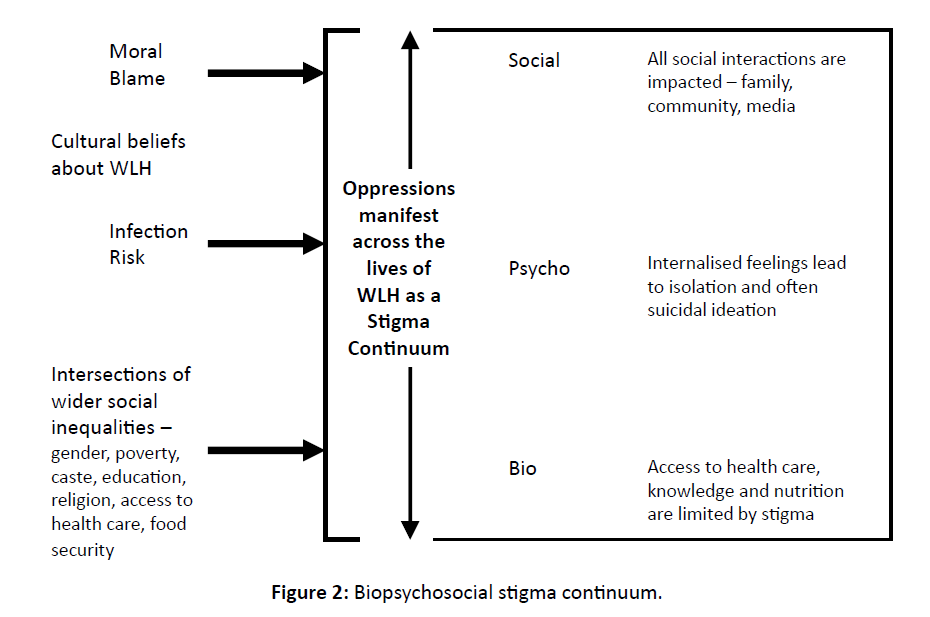
Although Ho and Holloway [2] and Parker and Aggleton
[17] identified the operation of HIV related stigma in both
public and private spheres, only Van Hollen [6] conceives
of a stigma continuum permeating all aspects of the life of a
WLH. It is proposed here that such a continuum is aligned
with Engel’s [19] biopsychosocial complex model. While
working with women and men with chronic disease, Engel [19]
noted that focussing exclusively on biomedical factors failed
to explain why some individual’s experienced debilitating
illness while others could manage their condition as a routine
problem to be addressed [20]. Considering each individual’s
experience from their particular perspective of living within the limits of their disease, Engel identified the criticality of social
relationships and psychological resilience [19]. While critiqued
as impractical in the clinical setting, Cohen and Forstein [21]
considered the approach vital to physicians developing a
compassionate and integrated approach to health care. Borrell-
Carrió et al. [22] argued that when considered for a defined
population, the biopsychosocial complex provided an important
perspective on the ways “…suffering, disease, and illness are
affected by multiple levels of organization, from the societal to
the molecular”.
Figure 1: Stigma continuum.
Also evaluating the effects of multiple levels of social
organization at the macro or group level, is the theory of
Intersectionality, an approach that considers how a group’s
place in social hierarchy is simultaneously constituted by
constructions including ethnicity, gender, class/ caste, religion
and age [23-25]. Recognising that stigma “feeds upon,
strengthens and reproduces existing inequalities of class, race,
gender and sexuality”, Rahangdale et al. [9] noted that Indian
cultural and historical institutions often stigmatise all women
with positive HIV sero-status [13]. Applying an intersectionality
lens to interpretation of the lived biopsychosocial experience of
particular clusters of Indian WLH, is suggested here as a means
for researchers to gain an over-view of the unequal social power
dynamics that result in a spectrum of biomedical, social and
psychological stigma manifestations for those groups of women.
Returning to the public: private dichotomy presented by Ho
and Holloway [2], Parker and Aggleton [17] and reimagining
it according to the biopsychosocial model, demonstrates that
WLH experience a whole-of-life stigma continuum (Figure 2).
As noted above, for Engel [19] the aim was for the physician
to work with the woman or man such that their chronic disease
would be experienced as a routine factor of life to be managed.
As can be seen in Figure 2 for a WLH or a population of WLH to
have the resources to experience HIV infection as a manageable chronic condition, would require overcoming stigma in every
context of life: biomedical/health care, psychological/personal
ideations, and social/relational interactions [19,26].
Women in India living an HIV: The pieces of a stigma
riddled life
Mitra and Sarkar [15] and Vlassoff et al. [13] report that
in India, a husband’s exposure to HIV commonly results from
having participated in high-risk heterosexual behaviours such
as having multiple sexual partners. Diagnosis then follows
development of advanced symptoms of AIDS, a related sexually
transmitted illness, or often after developing a comorbidity
with tuberculosis [18,14,27]. Vissandjeé et al. [28] and Sinha
et al. [14] note that while no consensus has been reached as
to causality, men typically have higher infection rates for
tuberculosis than women. Whether this relates to biological sex
related disease factors or results from social constructions of
gender, women’s reduced incidence of tuberculosis symptoms
with attendant tuberculosis and HIV testing and diagnosis means
that for women, one opportunity for HIV testing is removed and
diagnosis potentially delayed.
Unless tested for during pregnancy, HIV-positive
monogamous married women often remain undiagnosed until
their husband is terminally ill or deceased [4]. Many women
in South India, particularly poor rural women, are unaware of
the risk of HIV transmission from their husbands [6,15,26].
Furthermore, cultural and historical expectations of a wife’s
subordination to her husband mean that women often have little
control over marital sexual activity or safe-sex practices [12,26].
It is reported that HIV tests are often performed without the
woman’s consent, with results communicated to her husband’s
family, so, even after diagnosis the woman may not be advised
of her condition or receive treatment [1,6,15]. Family resources
are typically prioritised toward the husband’s care by the wife and the husband’s family [26]. While the wife may blame a
sex-worker for luring and infecting her husband, within the
family unit the wife herself is typically blamed for engaging
in immoral behaviour, infecting her husband and shaming his
family [6,9,26].
Figure 2: Biopsychosocial stigma continuum.
Entrenched patriarchal loyalty is rationalised by gendered
folk myths which connect a basic understanding of HIV
as transmitted in blood and sexual fluids, with traditional
cultural notions associating blood with impurity and death [6].
Van Hollen [6] described a gendered South Indian folk logic
which imagines menstruation as a means whereby women are
temporarily purged of the HIV virus, and which is claimed to
explain why husbands typically die before their wives. Van
Hollen [6] identified two social motives for accusing the wife
of introducing HIV: as protection of family honour by shifting
shame onto a scapegoat, and as justification for expelling the
‘aberrant widow’ and thereby avoiding the economic burden of
medical costs, child support and inheritance.
In rural communities there is little understanding of the
mechanisms and risks of virus transmission, and minimal
education about disease management [26]. Information is
instead gleaned from rumour, government statements, cultural
institutions and media [9]. Such a lack of accurate biomedical
knowledge, combined with widely held social perceptions
of HIV as an immoral, deadly, highly-contagious women’s
disease, generates fear and focuses shame on women, be they
sex-workers or wives [6,9].
Noting her husband’s diagnosis, and where not tested by the
family, to avoid the stigma of being known to be HIV-positive
WLH attempt to keep their HIV sero-status secret [15,18].
However secrecy often results in non-attendance for ARDT,
attempts to disguise symptoms, social isolation and women
travelling large distances on unreliable public transport to access care in remote centres with hopes of anonymity [18,29]. Regular
absences for treatment also take women away from the work of
caring for the family and incur travel costs, both of which may
further limit resources available to purchase medication and
nutrition [26]. On seeking care, many WLH meet disinterest,
fear of infection and moral condemnation at the hands of
medical staff [3,14,26,30]. Nyamathi et al. [26] and Rahangdale
et al. [9] both described WLH who experienced neglect, were
told that they were not worth treating as they would soon die,
were publicly shamed, and whose confidentiality was breached
by staff. However, it is also reported that such behaviour can
be reduced by engaging nursing staff in training to provide
infection information and opportunities to discuss concerns,
beliefs and behaviours [14,30].
The resources WLH can access to deal with daily stigma
directly affect their mental health [29]. Diagnosed with a
disease that is anecdotally understood to be immoral and fatal,
fearing stigma, and lacking both the education and support to
make informed choices about disclosing their HIV sero-status,
WLH in India report anxiety, depression and suicidal ideation
[1,18,26]. Depression is recognised as being a strong predictor
of poor ARDT adherence and declining quality of life [31].
Most married, monogamous WLH report that their internalised
stigma is associated with feeling that they have failed their
families by needing to receive care, rather than providing
care to the family as social roles teach that a woman should
[1,6,14,26,31]. To minimise the risk to their children, nursing
mothers reported implementing avoidant coping strategies,
eschewing maternal acts such as breastfeeding or touching their
infants, strategies which further reinforce feelings of maternal
failure [29]. Women also reported fearing that their children
would be ostracised and would have reduced opportunities for
education and a better future [9,26].
Stigmatised women: Looking up through an
intersectional biopsychosocial lens
This is the complex situation of the WLH: a world structured
by socially constructed notions of gender, defined by the
behaviours and relationships constituted appropriate for her as
a woman and a wife in Indian society, and inculcated by folk
beliefs and partial truths about a disease that will define the rest
of her life. And so her illness experience and disease progression
diverges from that of men in ways not predicted by biomedicine
alone.
In February 2017, The World Health Organisation’s
Human Reproduction Programme released a woman-centred
approach to care for women living with HIV [31]. Key to the
recommendations are involving WLH as “active participants
in, as well as beneficiaries of, trusted health systems that
respond to women’s needs, rights and preferences in humane
and holistic ways”, and the guideline provides a framework to
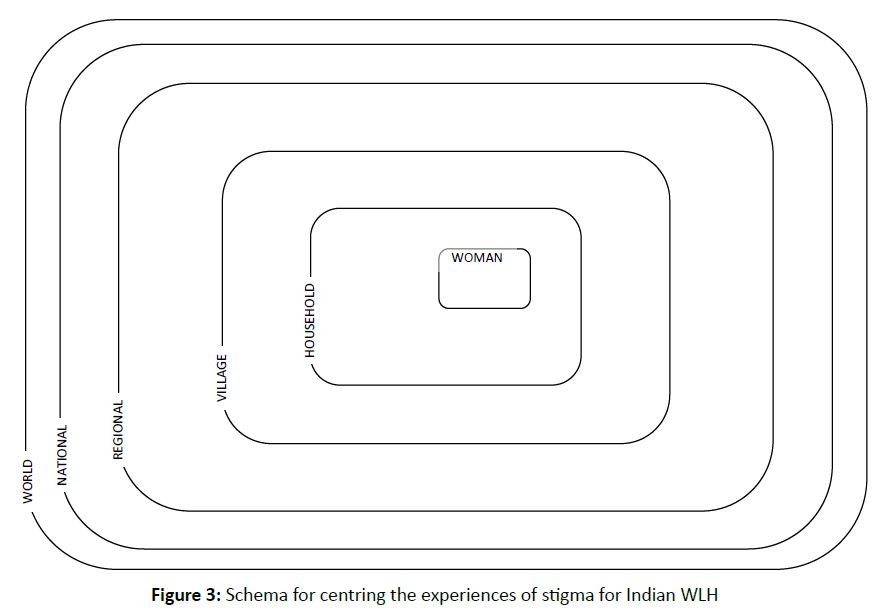
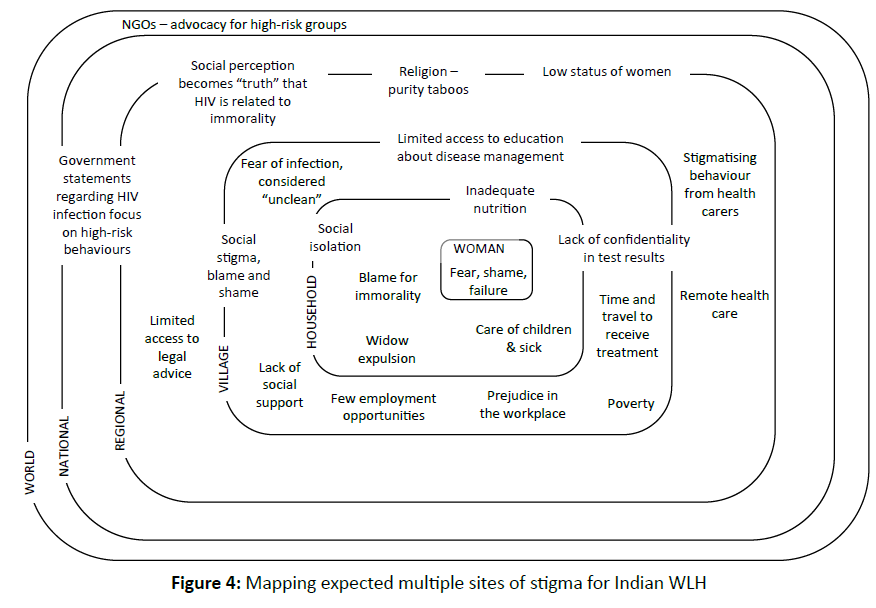
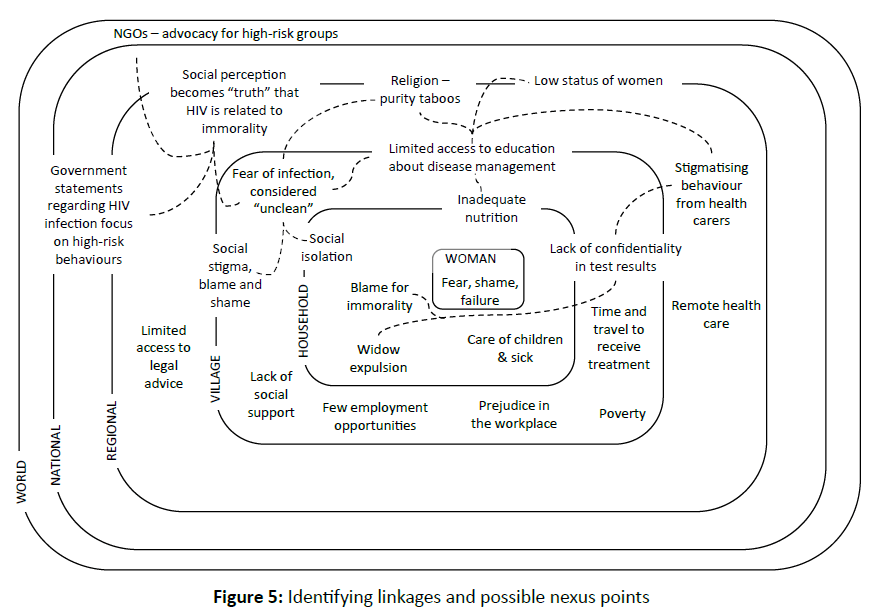
guide good practice. Developed for this paper, Figure 3 provides
one possible schema to allow researchers to map ethnographic
or qualitative questionnaire responses from a group of women
about experiences of stigma [32]. Once mapped as shown in Figure 4, common themes, clusters of stigma manifestations,
and potential root causes can be identified and linked as shown
in Figure 5, allowing further evaluation of opportunities to
maximize the effects of social change. In this way, the schema
proposed in Figures 3-6, becomes a means not only for mapping
reported experiences, but for identifying nexus points, and then
coordinating and prioritising care and assistance initiatives.
Figure 3: Schema for centring the experiences of stigma for Indian WLH.
Figure 4: Mapping expected multiple sites of stigma for Indian WLH.
Figure 5: Identifying linkages and possible nexus points.
Figure 6: Analysing Nyamathi et al [26] and mapping impacts for Indian WLH.
The findings of data analysis, and critical confirmation of the mapped results of questionnaires or ethnographic surveys,
could then be used to design multi-faceted systems of care. Such
systems would be inherently tailored to respond to specific,
identified sites of need and aim to reduce limits imposed by
stigma. A multi-faceted care program will respond not only to
daily tangible and biomedical needs of WLH, but also to provide
social and psychological support, and/or promote change in
social constructions of exclusion and poverty.
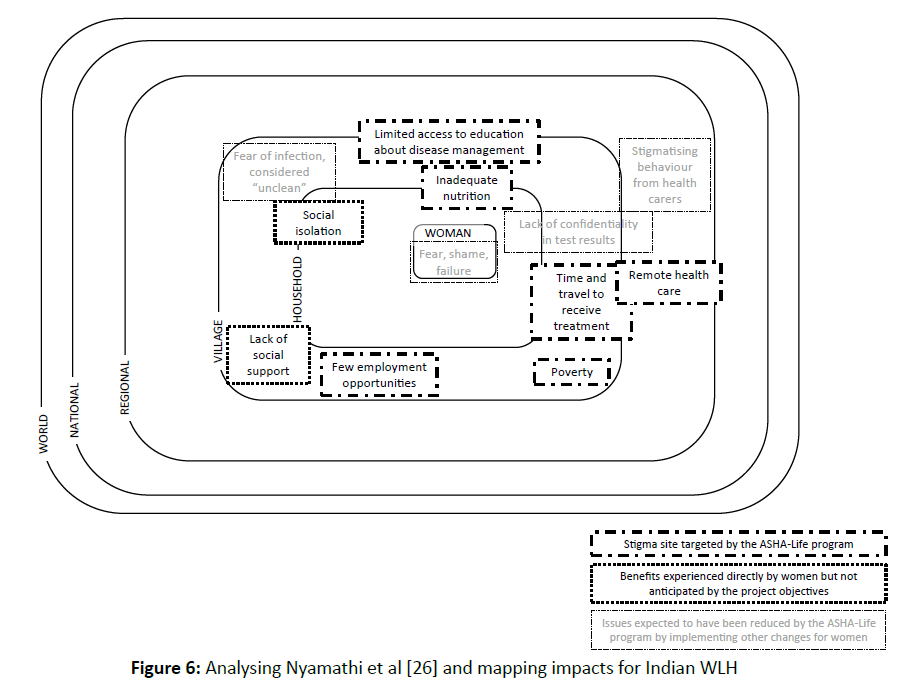
While not using the terminology of intersectionality, or a
biopsychosocial complex, the principles of this approach are
demonstrated in base-line research and an Asha-Life village
intervention reported by Nyamathi et al. [26,29,33]. In the most
recently reported focus group study [26], a group of 16 South
Indian, rural WLH met regularly with ASHA (Accredited Social
Health Activists), trained local advocates and were provided
with; transport to trusted medical therapy; tangible support
in the form of high protein food, cooking oil and money;
vocational training; and, education regarding management of
their condition. Based on the publication these initiatives are
mapped. In addition to achieving quantifiable health benefits,
the women who participated in the Asha-Life program stated
that the sense of community engendered was “powerful and
transformative” [26]. One participant said: “I am not thinking
that I am an AIDS patient. I just feel like [a] normal person”
and another: “I was not alone” [26]. The participants described
“improvements in their mood and their feelings of self-efficacy”
[26]. These additional benefits of the program are mapped in
Figure 6. While this intervention did not aim to directly change
the ideological social structures that so constrain WLH, it
demonstrated that coordinated attention to biomedical (treatment
and nutrition), psychological (counselling and empowerment),
and social (economic independence through skills development,
and belonging to a community) arenas generates real benefit in
improving women’s quality of life and health outcomes. This
initiative demonstrates that in order to achieve equitable health
outcomes, these particular WLH need care programs “which
emphasize nutritional knowledge, while reducing barriers to
receiving ART and [provide] physical, emotional, and financial
support” [26].
A biopsychosocial intersection: turning away from
stigma
While PLH around the world experience stigma and not all
PLH experience equity in accessing ARDT, women in India
who live with positive HIV sero-status are particularly engulfed
by stigma [3]. Employing Engel’s biopsychosocial model and
considering the intersection of mutually constitutive unequal
and inequitable power relations that limit a WLH life, allows
researchers to perceive the experience of stigma as a continuum
[19]. Stigma that otherwise forms a self-reinforcing hegemony
which separates WLH from ARDT and social support, reduces
their quality of life and increases the likelihood of terminal
illness outcomes and infection transmission [15]. Recognising
the interrelated nature of stigma suggests that single-point care
initiatives may do little to improve the overall quality of life
for WLH and instead tailored, multi-faceted approaches are
required.
In the complex context of establishing programs of care for
women living with HIV, arranging qualitative information on
lived experiences in such a way as to identify interacting barriers
to care, can assist in tailoring multifaceted HIV-care programs
that address the particular needs of specific groups of women.
Customised care programs aim: 1) to respond to the women’s
own identified and prioritised needs across biomedical, social
and psychological arenas in a coordinated manner, and 2) to effect social changes that result in a stigma laden environment.
The imperative to further develop, test and implement such
women-centred, multi-disciplined care initiatives originates in
an appreciation that HIV-related stigma is the greatest constraint
on the lives of almost one million Indian women today.
References
- Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, et al.(2012) Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India - a community based cross sectional study. BMC Public Health. 12: 463.
- Ho S, Holloway A (2016) The impact of HIVÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡ÃâÃÂrelated stigma on the lives of HIVÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡ÃâÃÂpositive women: An integrated literature review. J Clin Nurs. 25: 8-19.
- Kandwal R, Bahl T (2011) Link to slower access to care: What is the stigma? An Indian perspective. Curr HIV/AIDS Rep. 8: 235-240.
- MalavÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâé S, Ramakrishna J, Heylen E, Bharat S, Ekstrand ML, et al. (2014) Differences in testing, stigma, and perceived consequences of stigmatization among heterosexual men and women living with HIV in Bengaluru, India. AIDS Care. 26: 396-403.
- AIDS Data Hub: Evidence to action: Country Profile>India. (2016).
- Van Hollen C (2010) HIV/AIDS and the gendering of stigma in Tamil Nadu, South India. Culture, Medicine, and Psychiatry. 34: 633-57.
- The World Bank: HIV/AIDS in India (2012).
- Biradavolu MR, Blankenship KM, Jena A (2012) Structural stigma, sex work and HIV: Contradictions and lessons learnt from a community-led structural intervention in southern India. J. Epidemiol. Community Health.66: 95-99.
- Rahangdale L, Banandur P, Sreenivas A, Turan J, Washington R, et al. (2010) Stigma as experienced by women accessing prevention of parent-to-child transmission of HIV services in Karnataka, India. AIDS Care. 22: 836-842.
- Krishnan JK (2003) The rights of the new untouchables: A constitutional analysis of HIV jurisprudence in India. Hum Rights Q. 25: 791-819.
- Sharma N (2008) The new untouchables. In: Tribune India: Dehradun Plus Online Edition.
- Raj A, Saggurti N, Battala M, Nair S, Dasgupta A, et al. (2013) Randomized controlled trail to test the RHANI wives HIV intervention for women in India at risk for HIV from husbands. AIDS Behavior. 17: 3066-3080.
- Vlassoff C, Weiss MG, Rao S (2013) A question module for assessing community stigma towards HIV in rural India. J Biosoc Sci. 45: 359-74.
- Sinha G, Peters D, Bollinger R (2009) Strategies for gender-equitable HIV services in rural India. Health Policy Plan. 24: 197-208.
- Mitra A, Sarkar D (2011) Gender inequality and the spread of HIV-AIDS in India. IJSE. 38: 557-572.
- Goffman E (1991) Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster.
- Parker R, Aggleton P (2003) HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Soc. Sci. Med. 57: 13-24.
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, et al. (2008) HIV-related stigma: Adapting a theoretical framework for use in India. Soc. Sci. Med. 67: 1225-1235.
- Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science. 196: 129-136.
- Weston W (2005) Patient-Centered Medicine: A Guide to the Biopsychosocial Model. Fam Syst Health. 23: 387-392.
- Cohen M, Forstein A (2012) A Biopsychosocial Approach to HIV/AIDS Education for Psychiatry Residents. Acad Psychiatry. 36: 479-486.
- Borrell-CarriÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâó F, Suchman AL, Epstein RM2004) The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Ann Fam Med. 2: 576-82.
- Shields SA (2008) Gender: an intersectionality perspective. Sex Roles. 59: 301-311.
- Clark N, VissandjÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâée B (In Press) Gendered implications in the context of refugee resettlement: An intersectional analysis of language, (health) literacy and gender. InJordan-Zachery J, Hankivsky O (eds) Bringing Intersectionality to Public Policy.
- Hankivsky O (2012) WomenÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s health, menÃÆÃâÃââÃÆââ¬Å¡Ã¢ââ¬Å¡Ã¬ÃÆââ¬Å¡Ã¢ââ¬Å¾Ã¢s health, and gender and health: Implications of intersectionality. Soc. Sci. Med. 74: 1712-1720.
- Nyamathi A, Ekstrand M, Srivastava NCarpenter CL, Salem BE, et al. (2016) ASHA-Life intervention perspectives voiced by rural Indian women living with AIDS. Health Care Women Int.37: 412-425.
- Bloem M, Saadeh R (2010) Foreword: The role of nutrition and food insecurity in HIV and tuberculosis infections and the implications for interventions in resource-limited settings. Food Nutr Bull. 31: S 289-291.
- VissandjeÃÆÃâÃâ ââ¬â¢ÃÆââ¬Å¡Ãâé B, Mourid A, Greenaway CAShort WE, Proctor JA (2016) Searching for Sex- and Gender-sensitive Tuberculosis Research in Public Health: Finding a Needle in a Haystack. Int. J. Wom. Health. 8: 731-42.
- Nyamathi A, Ekstrand M, Salem BE (2013) Impact of ASHA intervention on stigma among rural Indian women with AIDS. WJNR. 35: 867-883.
- Shah SM, Heylen E, Srinivasan K, Perumpil S, Ekstrand ML, et al. (2014) Reducing HIV stigma among nursing students: A brief intervention. WJNR. 36: 1323-1337.
- Mohite VR, Mohite RV, George J (2015) Correlates of perceived stigma and depression among the women with HIV/AIDS infection. BJMS. 14: 151-158.
- World Health Organisation: Consolidated Guideline on sexual and reproductive health and rights of women living with HIV (2017).
- Nyamathi A, Ekstrand M, Zolt-Gilburne J, Ganguly K, Sinha S, et al. (2011) Correlates of Stigma among Rural Indian Women Living with HIV/AIDS. AIDS and Behavior. 17: 329-339.